
Carbon monoxide causes hypoxia by forming carboxyhemoglobin and shifting the oxyhemoglobin dissociation curve to the left. However, the brain and heart with high metabolic rate are most susceptible to it. Every organ in human body could be damaged due to CO poisoning. Patients usually do not recognize the fact that they were exposed to CO. Mild exposure to CO causes headache, myalgia or dizziness whereas severe exposure will result in confusion, loss of consciousness or death. The symptoms of CO poisoning are non-specific. Breaking-up (17.8%), financial debt (17.8%), and physical/mental illnesses (17.8%) were the top three reasons for committing suicide. In a preliminary study at the Chang Gung Memorial Hospital, it was reported that most patients that attempted suicide by charcoal burning had underlying major depressive (49.3%) or adjustment (41.1%) disorders. Charcoal burning soon became the second most common method of suicide and led to a 20% increase in the overall suicide rate. During the same period, the incidence of suicide by charcoal burning alone had multiplied by nearly 25-fold, which is from 0.22 to 5.4 for every 100,000 people in Taiwan. For example, the ratio of national suicide rate from 1999 to 2009 in Taiwan had increased from 10.4 to 19.3 for every 100,000 people. First reported in Hong Kong in 1998, suicide by charcoal burning has had an epidemic spread in Asia. The CO poisoning can be intentionally utilized as a form of suicide by burning charcoal and exposing themselves to the smoke. Indeed, between 19, there was a significant increase in the rate of unintentional deaths from CO poisoning in Taiwan (i.e., from 1.6 to 3.5 per 10 6 person-years).

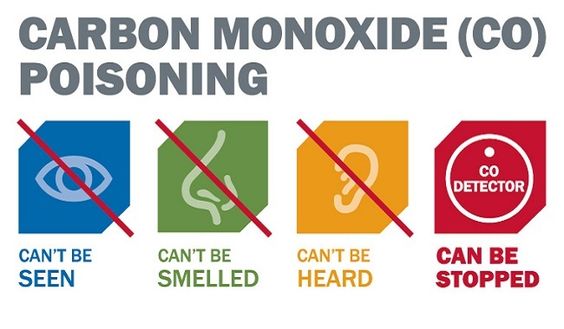
The most common sources of unintentional CO poisoning are faulty or inadequately ventilated gas heating appliances, fires, and automobile exhaust fumes. CO is an odorless gas formed during an incomplete combustion of organic material. Finally, Kaplan-Meier analysis confirmed that patients with shock suffered greater cumulative mortality than without shock (Log-rank test, Chi-square 147.404, P<0.001).Ĭarbon monoxide (CO) toxicity is common in Taiwan. In a multivariate-Cox-regression model, it was revealed that shock status was a significant predictor for mortality after carbon monoxide poisoning (OR 8.696, 95% CI 2.053-37.370, P=0.003). However, hyperbaric oxygen therapy was only used in 18.8% of the patients. All patients were treated with high concentration of oxygen therapy using non-rebreather mask. Furthermore, the non-survivors suffered greater incidences of hypothermia (P<0.001), respiratory failure (P<0.001), shock (P<0.001), hepatitis ((P=0.016), renal failure (P=0.003), coma (P<0.001) than survivors. Carbon monoxide produced many serious complications after exposure: fever (26.1%), hypothermia (9.6%), respiratory failure (34.1%), shock (8.4%), myocardial infarction (8.0%), gastrointestinal upset (34.9%), hepatitis (18.4%), renal failure (25.3%), coma (18.0%) and rhabdomyolysis (21.8%). Most of the patients were middle-aged adults (33☑9 years), and were referred to our hospital in a relatively short period of time (6☑0 hours). Approximately half of the cases (49.4%) attempted suicide by burning charcoal.


 0 kommentar(er)
0 kommentar(er)
